Christinamh
Member Since 2024
Hi, my name is Christina. My cats name is Presley. This is my first post on this forum. This post will be long. Please bear with me. I am in desperate need of advice right now.
Presley is 12 years old (domestic shorthair) and first diagnosed with diabetes on 9/11/23. He started on 1 unit of prozinc on the same day.
On 1/2/24 he had an fructosamine test and his insulin was lowered to 0.5 units but I was told if I saw him eating, drinking, and urinating more often to increase back up to 1 unit. A couple weeks later I did increase back up to 1 unit.
On 4/2/24 he had a fructosamine and full bloodwork done. Bloodwork showed no abnormalities. His fructosamine was high and I was told to increase his insulin to 2 units.
2 days later we lost his brother Theodore to cancer. We were also in the process of moving. It was a stressful time for Presley.
On 4/23/24 he had another fructosamine test to ensure he should stay on 2 units. The vet told me at that time to continue on 2 units.
On 5/7/24 he was seen by his primary care vet for itchy ears. They initially thought it was an infection. Prescribed medicated drops. It did not get better. He had a follow up on 5/21/24 and it was concluded that he did not have an infection, but rather the itchy ears were allergy related (he has struggled with chronic rhinitis—pretty severe—for 4 years now). He was prescribed cyclosporine, 0.3ml once a day. It has completely alleviated the rhinitis and inflammation in his nose. First time in 4 years he has been able to breath normally.
Let me preface this next part with this; his primary vet told me his diet (natures variety instinct limited ingredient rabbit raw coated kibble to graze through out the day, wet/canned version at feeding times before insulin, or rawz 96% rabbit at feeding time). My vet also never discussed doing blood glucose readings. When he was first diagnosed they told me they could be a sensor on him to monitor the levels but didn’t recommend it as I would probably drive myself crazy reading the numbers.
When he was put on cyclosporine 5 weeks ago I’d say I noticed somewhat of a difference in his eating habits. He was eating less. Not significantly less and definitely not skipping meals, but less. Instead of eating a half can of food at feeding time, he’d eat a quarter. But he’d always follow up with a little dry food. I’d say over the last 2 weeks it has been most noticeable. I’ll say I’ve also noticed a decrease in his energy. I didn’t think a whole lot of it, kind of chalked it up to old age maybe. Or maybe I was just being paranoid.
This past Saturday night (6/22/24) after feeding and getting insulin (about 2 hours later) he was acting very strange. He threw up what looked like some whole dry food and bile. This is very out of the norm for Presley as he has only ever thrown up twice in his whole life. He also started ravenously eating and drinking. He started walking around and was a little vocal and just looked confused. I rushed him to the ER. He was considered to be in hypoglycemia. His glucose was at 66. He was given a dextrose IV and a cerenia injection. They installed a freestyle libre monitor. I was told to at least cut his insulin in half and if I didn’t feel comfortable with that than to give a half unit. I was told not to let his glucose go below 100 and to offer small meals through out the night. The doctor and tech both told me it was very possible he was in remission.
Sunday (6/23) at 6am he got a full meal and half a unit of insulin. During the day his levels kept falling below 100, to 90-95. I would offer food and be would eat and they would come back up. But I had to offer food every hour to keep his levels above 100. I suspected he didn’t need the insulin. Normally he would not eat every hour like this but I think the cerenia was allowing for the increased appetite. He was also overly tired all day. Barely left the bed. Just wanted to sleep.
Monday (6/24) I made the judgment call (probably stupid on my part) to skip his morning insulin. He was back to himself fully. Normal energy and acting normal. His glucose numbers were normal. They remained normal all day. A little high between 10am-12pm (180-200) but came back down to 112-150 through out the rest of the day. Unfortunately I can’t keep myself from checking all the time.
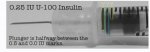
I made a phone call to my primary vet to see how they wanted to proceed. Unfortunately my primary vet is on vacation until Saturday. She just brought on a second doctor who Presley has never seen before. I spoke with her and got really conflicting information. She told me to continue giving half a unit of insulin. She told me to completely take away his dry food and only feed him twice a day. She told me there was no concern if his numbers were below 100 as long as they didn’t go below 80. I told her I just couldn’t offer food every hour to try to get him above 100 should they drop with insulin. His glucose had also remained normal all day without the insulin in the morning (this was at 4:30pm). She told me to stick to giving half a unit. I told her that ER doctors suspected Presley has gone into remission. She told me that would be impossible to tell right now. I just didn’t feel comfortable with our conversation. She was giving me conflicting information at certain points in the conversation. For example, completely take away his dry food. He’s had dry food his whole life and has grazed his whole life. I don’t think I could make that sudden of a change. I asked her what to do if I couldn’t get him to eat canned/wet food (lately he has been refusing it). She told me then I could offer some dry food but at that point to only give half a dose of insulin which would be half of a half unit. I don’t even know how I’m supposed to measure that. The ER doctor said not to bother trying to give half of a half unit as that’s like trying to measure a drop. Something about our whole conversation just didn’t feel right.
Anyway, I fed him at his normal feeding time (6pm). He would not touch canned/wet food at all. I tried 3 different things. He didn’t want it. So I offered dry food and he ate a decent amount. So per the vets instructions I gave a half unit of insulin. I still just wasn’t feeling comfortable with our conversation. So I took him back to ER just to be able to talk to the doctors on staff there (it’s a state of the art facility with some of the best doctors I’ve ever met. They have way more than most ERs with multiple specialists on staff 24hrs). They ended up doing a fructosamine and urinalysis to determine if he was in remission. His fructosamine came back at 315 (just above their threshold for remission at 300 or below) and the urinalysis showed no glucose or ketones in the urine at all. The doctor said we’re not totally out of the woods but that it does seem like he is likely in remission and recommended stopping the insulin. She also recommended that I change his food because he cannot have raw while he is on cyclosporine because it increases his chances of infection (something my primary never discussed with me). She said dry food was fine. She gave me a bag of hill’s prescription diet multi-benefit w/d.
We got home at about 9:30pm EST and I did offer him some dry food to see if he would eat the new food. He did eat some. Not a whole lot, but some. And he drank some water. His glucose level per the freestyle sensor was at 215. The highest it has been since getting the monitor. I chalked it up to stress. I went to bed. I woke up at 11:45 and it was at 225.
Finally here is where things go array. At 2:21am his levels were at 274 with an up arrow (indicating they were going up). Naturally I’m freaking out. I continue to scan the monitor every couple minutes even though I know I should not. At 2:45am his levels were at 297. I called the ER. I spoke with a nurse who said that still wasn’t dangerously high. They came down a little in 10 minutes to 270. She said to continue monitoring and to call if they went over 300. She said to still not give insulin. And this is where I’m not sure what to do. As of 4:15am his glucose level is at 256 with a straight arrow.
I know that no one here is a doctor, but I have now gotten two different answers from 2 different doctors. I hate that his primary care doctor is on vacation. However, the doctors at this specific ER have always seemed so “advanced” and to really know what they’re doing and talking about. I just don’t know whether I should give a half unit at 6am or not to give. His numbers have not been this high (or even close to it) since he got the freestyle. To clarify, I did give insulin as instructed Sunday at 6am and 6pm. I skipped the dose Monday morning at 6am. However at 6pm on Monday he did get half a unit. Can someone please help. I am just desperate at this point. The ER doctor did mention not letting his levels go above 300 because you risk ketoacidosis and after a quick google search it scares the crap out of me. Please can offer any advice?
edit: it is 4:45am and his levels right now read 234 with a straight arrow.
Presley is 12 years old (domestic shorthair) and first diagnosed with diabetes on 9/11/23. He started on 1 unit of prozinc on the same day.
On 1/2/24 he had an fructosamine test and his insulin was lowered to 0.5 units but I was told if I saw him eating, drinking, and urinating more often to increase back up to 1 unit. A couple weeks later I did increase back up to 1 unit.
On 4/2/24 he had a fructosamine and full bloodwork done. Bloodwork showed no abnormalities. His fructosamine was high and I was told to increase his insulin to 2 units.
2 days later we lost his brother Theodore to cancer. We were also in the process of moving. It was a stressful time for Presley.
On 4/23/24 he had another fructosamine test to ensure he should stay on 2 units. The vet told me at that time to continue on 2 units.
On 5/7/24 he was seen by his primary care vet for itchy ears. They initially thought it was an infection. Prescribed medicated drops. It did not get better. He had a follow up on 5/21/24 and it was concluded that he did not have an infection, but rather the itchy ears were allergy related (he has struggled with chronic rhinitis—pretty severe—for 4 years now). He was prescribed cyclosporine, 0.3ml once a day. It has completely alleviated the rhinitis and inflammation in his nose. First time in 4 years he has been able to breath normally.
Let me preface this next part with this; his primary vet told me his diet (natures variety instinct limited ingredient rabbit raw coated kibble to graze through out the day, wet/canned version at feeding times before insulin, or rawz 96% rabbit at feeding time). My vet also never discussed doing blood glucose readings. When he was first diagnosed they told me they could be a sensor on him to monitor the levels but didn’t recommend it as I would probably drive myself crazy reading the numbers.
When he was put on cyclosporine 5 weeks ago I’d say I noticed somewhat of a difference in his eating habits. He was eating less. Not significantly less and definitely not skipping meals, but less. Instead of eating a half can of food at feeding time, he’d eat a quarter. But he’d always follow up with a little dry food. I’d say over the last 2 weeks it has been most noticeable. I’ll say I’ve also noticed a decrease in his energy. I didn’t think a whole lot of it, kind of chalked it up to old age maybe. Or maybe I was just being paranoid.
This past Saturday night (6/22/24) after feeding and getting insulin (about 2 hours later) he was acting very strange. He threw up what looked like some whole dry food and bile. This is very out of the norm for Presley as he has only ever thrown up twice in his whole life. He also started ravenously eating and drinking. He started walking around and was a little vocal and just looked confused. I rushed him to the ER. He was considered to be in hypoglycemia. His glucose was at 66. He was given a dextrose IV and a cerenia injection. They installed a freestyle libre monitor. I was told to at least cut his insulin in half and if I didn’t feel comfortable with that than to give a half unit. I was told not to let his glucose go below 100 and to offer small meals through out the night. The doctor and tech both told me it was very possible he was in remission.
Sunday (6/23) at 6am he got a full meal and half a unit of insulin. During the day his levels kept falling below 100, to 90-95. I would offer food and be would eat and they would come back up. But I had to offer food every hour to keep his levels above 100. I suspected he didn’t need the insulin. Normally he would not eat every hour like this but I think the cerenia was allowing for the increased appetite. He was also overly tired all day. Barely left the bed. Just wanted to sleep.
Monday (6/24) I made the judgment call (probably stupid on my part) to skip his morning insulin. He was back to himself fully. Normal energy and acting normal. His glucose numbers were normal. They remained normal all day. A little high between 10am-12pm (180-200) but came back down to 112-150 through out the rest of the day. Unfortunately I can’t keep myself from checking all the time.
I made a phone call to my primary vet to see how they wanted to proceed. Unfortunately my primary vet is on vacation until Saturday. She just brought on a second doctor who Presley has never seen before. I spoke with her and got really conflicting information. She told me to continue giving half a unit of insulin. She told me to completely take away his dry food and only feed him twice a day. She told me there was no concern if his numbers were below 100 as long as they didn’t go below 80. I told her I just couldn’t offer food every hour to try to get him above 100 should they drop with insulin. His glucose had also remained normal all day without the insulin in the morning (this was at 4:30pm). She told me to stick to giving half a unit. I told her that ER doctors suspected Presley has gone into remission. She told me that would be impossible to tell right now. I just didn’t feel comfortable with our conversation. She was giving me conflicting information at certain points in the conversation. For example, completely take away his dry food. He’s had dry food his whole life and has grazed his whole life. I don’t think I could make that sudden of a change. I asked her what to do if I couldn’t get him to eat canned/wet food (lately he has been refusing it). She told me then I could offer some dry food but at that point to only give half a dose of insulin which would be half of a half unit. I don’t even know how I’m supposed to measure that. The ER doctor said not to bother trying to give half of a half unit as that’s like trying to measure a drop. Something about our whole conversation just didn’t feel right.
Anyway, I fed him at his normal feeding time (6pm). He would not touch canned/wet food at all. I tried 3 different things. He didn’t want it. So I offered dry food and he ate a decent amount. So per the vets instructions I gave a half unit of insulin. I still just wasn’t feeling comfortable with our conversation. So I took him back to ER just to be able to talk to the doctors on staff there (it’s a state of the art facility with some of the best doctors I’ve ever met. They have way more than most ERs with multiple specialists on staff 24hrs). They ended up doing a fructosamine and urinalysis to determine if he was in remission. His fructosamine came back at 315 (just above their threshold for remission at 300 or below) and the urinalysis showed no glucose or ketones in the urine at all. The doctor said we’re not totally out of the woods but that it does seem like he is likely in remission and recommended stopping the insulin. She also recommended that I change his food because he cannot have raw while he is on cyclosporine because it increases his chances of infection (something my primary never discussed with me). She said dry food was fine. She gave me a bag of hill’s prescription diet multi-benefit w/d.
We got home at about 9:30pm EST and I did offer him some dry food to see if he would eat the new food. He did eat some. Not a whole lot, but some. And he drank some water. His glucose level per the freestyle sensor was at 215. The highest it has been since getting the monitor. I chalked it up to stress. I went to bed. I woke up at 11:45 and it was at 225.
Finally here is where things go array. At 2:21am his levels were at 274 with an up arrow (indicating they were going up). Naturally I’m freaking out. I continue to scan the monitor every couple minutes even though I know I should not. At 2:45am his levels were at 297. I called the ER. I spoke with a nurse who said that still wasn’t dangerously high. They came down a little in 10 minutes to 270. She said to continue monitoring and to call if they went over 300. She said to still not give insulin. And this is where I’m not sure what to do. As of 4:15am his glucose level is at 256 with a straight arrow.
I know that no one here is a doctor, but I have now gotten two different answers from 2 different doctors. I hate that his primary care doctor is on vacation. However, the doctors at this specific ER have always seemed so “advanced” and to really know what they’re doing and talking about. I just don’t know whether I should give a half unit at 6am or not to give. His numbers have not been this high (or even close to it) since he got the freestyle. To clarify, I did give insulin as instructed Sunday at 6am and 6pm. I skipped the dose Monday morning at 6am. However at 6pm on Monday he did get half a unit. Can someone please help. I am just desperate at this point. The ER doctor did mention not letting his levels go above 300 because you risk ketoacidosis and after a quick google search it scares the crap out of me. Please can offer any advice?
edit: it is 4:45am and his levels right now read 234 with a straight arrow.