Cal & Candy
Member Since 2024
Candy is our 13-ish year old female. We've had her about a year and a half. She currently has stage-2 kidney disease, a hyper-active thyroid, diabetes and acromegaly. This is our introduction.

Since Candy has multiple health issues, I thought it might be useful to give a summary of her medical history. I apologize in advance for the length; feel free to skip over it. I have several questions at the bottom about continuous glucose monitor (CGM) placement and retention; please look those over if you know about CGMs.
Medical History
CGM Questions:
· PLACEMENT: What are good CGM locations? Candy’s first (and only) CGM was placed on her right side, about over her front paw when standing and about 2 inches from the spine. That puts it right over the “crease” at the base of her neck when she’s on her side, with her head up; it seems like it needs to go farther back. How close to the spine can it go? How often can a location be reused?
· ADHESIVE: What supplemental adhesives are people using for CGMs?
· ADHESIVE REMOVER: What do you use to remove the sensor and/or residual adhesive?
· OVER-BANDAGE: What are people’s experiences with over-bandages, to keep the kitty from tearing off the sensor?
· PROTECTIVE VEST: Has anyone found a good vest to protect a CGM? Searches so far turn up “Thunder Vests” (too heavy), “recovery suits” that go over all four legs (too long), and assorted costumes. I’m looking for a light-weight vest-type garment with a Velcro (preferred) or zipper closure in the back that can be worn for extended periods,
Thanks!
Cal
Since Candy has multiple health issues, I thought it might be useful to give a summary of her medical history. I apologize in advance for the length; feel free to skip over it. I have several questions at the bottom about continuous glucose monitor (CGM) placement and retention; please look those over if you know about CGMs.
Medical History
We adopted Candy at the end of February, 2023. She had not been getting regular vet care when we adopted her, and her previous owner couldn't remember when her last visit to the vet was. At that time she appeared healthy, weighed 9.3 pounds and appeared to be slightly heavy for her size. She had been fed only dry food for her entire life.
Our first vet visit revealed that she had a urinary tract infection (UTI). We went through several courses of antibiotics to treat the UTI. It would clear up, then pop back up a month or so later.
By mid-July, she had lost over a pound of weight. She stopped eating, became lethargic and began vomiting so we took her into the emergency vet. They found that she was dehydrated, constipated and appeared to have kidney disease. An X-ray showed that she had only one kidney, pprobably from birth.
In August, she was diagnosed with chronic kidney disease, IRIS stage 2. We switched to a renal support diet.
By mid October, her weight was down to 7.5 pounds. We started giving her 1/8 tablet (by weight, about 1.9mg) mirtazipine (MIR) every 48 hours (QOD). We continued the MIR for one month; I don't recall exactly why it was discontinued, probably because of the way it was affecting her.
Her annual exam in February, 2024 revealed another UTI and that she had a hyper-active thyroid. We began giving her methimazole twice daily (bid) for hyperthyroidism. Her weight was still around 7.5 pounds. A course of amoxicillin clavulanate failed to clear up the UTI. A follow-up course of ciprofloxacin HCl seems to have finally cleared up her UTIs.
For several months her weight stayed between 7.5 and 7.7 pounds. She was drinking 3-5oz of water and eating 0.3-0.8oz dry and 0.6-0.9oz canned food. In early July, her weight dropped to 7.5 pounds and she was drinking and eating less than normal. I gave her a single 1/8 tablet dose of MIR and we started coating her dry food with Hartz Delectables Bisque. Her appetite rallied and she was suddenly consuming 8-10oz of water, 1.0-1.8oz dry and about 1oz of canned food. What's remarkable here is that this seems to be the point where she developed diabetes. We took her to the vet a week later and testing showed that she had diabetes.
The vet prescribed 1.0U Lantose glargine insulin (INS) bid and told us to come in for a fructosamine check in 3 weeks; we switched to a diabetic diet (Hill’s M/D). Our friends had recently lost a kitty to diabetes (beautiful, timid Timmie), so we did some research and decided that we needed to do home blood glucose (BG) testing. (The vet had NOT suggested this....)
We picked up a Contour Next tester, etc., and did our first curve a week after starting INS. Candy's BG tested 272 (mg/dl) at 1200 (24-hour time), dropped to 173 at 1800 and topped out at 347 at 2400. (All BG testing done from rear paw pads.) Based on that curve, the vet had us increase INS to 1.5 bid. Checks 24 hours later read: 316 at 1200, 283 at 1600, 273 at 1800. Being new to this, I figured we were OK. Six days after the increased dose we did another curve. This time she started at 147 at 1200, dropped to 49 at 1600 and came back up to 181 at 2000. As soon as we got the 49 reading (followed with a second test of 47 a few minutes later) we called the vet and she had us change the INS to 1.5U at 1200, 1.0U at 2400.
I continued to do BG tests at 1200, 1600 and 1800 for several days, then dropped the 1800 test. The lowest four-hour reading was a low of 284 at 1200 dropping to 223; the highest reading was 479 at 1200 dropping to 388. The 4-hour drop was fairly consistent, ranging from 40 to 70 mg/dl, mostly starting between 300 and 420 at 1200. Three weeks after changing the INS dose we went in for a fructosamine test and I showed the vet my BG data. She began to suspect acromegaly and ordered aldosterone and insulin-like growth factor tests.
On 9/4, the vet called with a diagnosis of acromegaly, increased INS to 2.0U bid, and we started giving MIR QOD. Testing at 1200, 1600 and 2400 didn't seem to show much improvement. BG ranged from 410 to 280, occasionally going higher.
On 9/11, we were concerned about Candy's breathing when resting and took her to the vet. I showed the vet my latest BG numbers and she increased INS to 2.5U bid. We reduced the MIR to 1.0mg QOD. (I grind up the MIR tablet, discard the flakes of enteric coating and weigh out the dose using a 1mg scale.) The increased INS was finally able to intermittently bring BG into the normal range. The lower dose of MIR still stimulated her appetite but without making her hyperactive.
Over the next several days, I began to notice that on MIR days, Candy’s BG spent more time in the normal range. On 9/21, I accidentally gave her MIR after only 24 hours and she spent most of the time in range.
On 9/25, Candy’s 1200 GB was 55. I called the vet and she told me to only give 2.5U INS if BG over 100, 1.0U if under 100 and to hold INS if under 60. She recommended we install a CGM (which took several days to set up). We also went to daily doses of 1.0mg MIR, given at 1200.
The daily MIR seemed to make a huge difference. Over the next week Candy’s BG typically ranged between 70 and 120, with occasional extremes of 58 to 158. I typically dosed 2.5U @1200 and 1.0U at 2400.
On 10/3, we went in for a tech appointment to place an Abbot Freestyle Libre 3 plus CGM. The vet was too busy to talk to us or look at my BG data; supposedly she would look it over later and call…. We were told to give 2.5U INS bid. Against my better judgment, I gave 2.5U at 0035 that night. An hour later the Libre gave a low glucose alarm with a BG of 55. I did a paw stick ten minutes later and got BG of 62 (CGM reading 64). Candy showed no clinical signs of hypoglycemia (hypo). I stayed up with her all night. She spent most of the next 3 hours in the hypo range and was in and out of it for about 12 hours. I skipped the 1200 INS dose and we finally got her back under control 18 hours after the 2.5U dose.
The vet told us to drop the INS dose to 2.0U bid, but I ignored that and gave alternating doses of 1.0 and 1.5U, depending on the Libre data, for the lifetime of the sensor (8 days). On day 8, I walked away for 10 minutes and returned to find Candy in her bed and the sensor on the floor. Prior to that, she hadn’t seemed to pay attention to it and it appeared to be securely adhered. I’ve attached Candy’s LibreView Weekly Summary and Glucose Profile charts for anyone who’s interested.
Since losing the sensor, I’ve been doing paw prick BG tests at 1200 & 2400. BG readings have mostly been 106 and 142, with one outlier of 187. I’m giving alternating doses of 1.0 and 1.5U INS.
Once we resumed MIR a month ago, Candy’s weight began to improve. Daily 1.0mg doses worked better than QOD. She’s now up to about 9.4 pounds, slightly more than when we adopted her.
Our first vet visit revealed that she had a urinary tract infection (UTI). We went through several courses of antibiotics to treat the UTI. It would clear up, then pop back up a month or so later.
By mid-July, she had lost over a pound of weight. She stopped eating, became lethargic and began vomiting so we took her into the emergency vet. They found that she was dehydrated, constipated and appeared to have kidney disease. An X-ray showed that she had only one kidney, pprobably from birth.
In August, she was diagnosed with chronic kidney disease, IRIS stage 2. We switched to a renal support diet.
By mid October, her weight was down to 7.5 pounds. We started giving her 1/8 tablet (by weight, about 1.9mg) mirtazipine (MIR) every 48 hours (QOD). We continued the MIR for one month; I don't recall exactly why it was discontinued, probably because of the way it was affecting her.
Her annual exam in February, 2024 revealed another UTI and that she had a hyper-active thyroid. We began giving her methimazole twice daily (bid) for hyperthyroidism. Her weight was still around 7.5 pounds. A course of amoxicillin clavulanate failed to clear up the UTI. A follow-up course of ciprofloxacin HCl seems to have finally cleared up her UTIs.
For several months her weight stayed between 7.5 and 7.7 pounds. She was drinking 3-5oz of water and eating 0.3-0.8oz dry and 0.6-0.9oz canned food. In early July, her weight dropped to 7.5 pounds and she was drinking and eating less than normal. I gave her a single 1/8 tablet dose of MIR and we started coating her dry food with Hartz Delectables Bisque. Her appetite rallied and she was suddenly consuming 8-10oz of water, 1.0-1.8oz dry and about 1oz of canned food. What's remarkable here is that this seems to be the point where she developed diabetes. We took her to the vet a week later and testing showed that she had diabetes.
The vet prescribed 1.0U Lantose glargine insulin (INS) bid and told us to come in for a fructosamine check in 3 weeks; we switched to a diabetic diet (Hill’s M/D). Our friends had recently lost a kitty to diabetes (beautiful, timid Timmie), so we did some research and decided that we needed to do home blood glucose (BG) testing. (The vet had NOT suggested this....)
We picked up a Contour Next tester, etc., and did our first curve a week after starting INS. Candy's BG tested 272 (mg/dl) at 1200 (24-hour time), dropped to 173 at 1800 and topped out at 347 at 2400. (All BG testing done from rear paw pads.) Based on that curve, the vet had us increase INS to 1.5 bid. Checks 24 hours later read: 316 at 1200, 283 at 1600, 273 at 1800. Being new to this, I figured we were OK. Six days after the increased dose we did another curve. This time she started at 147 at 1200, dropped to 49 at 1600 and came back up to 181 at 2000. As soon as we got the 49 reading (followed with a second test of 47 a few minutes later) we called the vet and she had us change the INS to 1.5U at 1200, 1.0U at 2400.
I continued to do BG tests at 1200, 1600 and 1800 for several days, then dropped the 1800 test. The lowest four-hour reading was a low of 284 at 1200 dropping to 223; the highest reading was 479 at 1200 dropping to 388. The 4-hour drop was fairly consistent, ranging from 40 to 70 mg/dl, mostly starting between 300 and 420 at 1200. Three weeks after changing the INS dose we went in for a fructosamine test and I showed the vet my BG data. She began to suspect acromegaly and ordered aldosterone and insulin-like growth factor tests.
On 9/4, the vet called with a diagnosis of acromegaly, increased INS to 2.0U bid, and we started giving MIR QOD. Testing at 1200, 1600 and 2400 didn't seem to show much improvement. BG ranged from 410 to 280, occasionally going higher.
On 9/11, we were concerned about Candy's breathing when resting and took her to the vet. I showed the vet my latest BG numbers and she increased INS to 2.5U bid. We reduced the MIR to 1.0mg QOD. (I grind up the MIR tablet, discard the flakes of enteric coating and weigh out the dose using a 1mg scale.) The increased INS was finally able to intermittently bring BG into the normal range. The lower dose of MIR still stimulated her appetite but without making her hyperactive.
Over the next several days, I began to notice that on MIR days, Candy’s BG spent more time in the normal range. On 9/21, I accidentally gave her MIR after only 24 hours and she spent most of the time in range.
On 9/25, Candy’s 1200 GB was 55. I called the vet and she told me to only give 2.5U INS if BG over 100, 1.0U if under 100 and to hold INS if under 60. She recommended we install a CGM (which took several days to set up). We also went to daily doses of 1.0mg MIR, given at 1200.
The daily MIR seemed to make a huge difference. Over the next week Candy’s BG typically ranged between 70 and 120, with occasional extremes of 58 to 158. I typically dosed 2.5U @1200 and 1.0U at 2400.
On 10/3, we went in for a tech appointment to place an Abbot Freestyle Libre 3 plus CGM. The vet was too busy to talk to us or look at my BG data; supposedly she would look it over later and call…. We were told to give 2.5U INS bid. Against my better judgment, I gave 2.5U at 0035 that night. An hour later the Libre gave a low glucose alarm with a BG of 55. I did a paw stick ten minutes later and got BG of 62 (CGM reading 64). Candy showed no clinical signs of hypoglycemia (hypo). I stayed up with her all night. She spent most of the next 3 hours in the hypo range and was in and out of it for about 12 hours. I skipped the 1200 INS dose and we finally got her back under control 18 hours after the 2.5U dose.
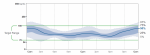
The vet told us to drop the INS dose to 2.0U bid, but I ignored that and gave alternating doses of 1.0 and 1.5U, depending on the Libre data, for the lifetime of the sensor (8 days). On day 8, I walked away for 10 minutes and returned to find Candy in her bed and the sensor on the floor. Prior to that, she hadn’t seemed to pay attention to it and it appeared to be securely adhered. I’ve attached Candy’s LibreView Weekly Summary and Glucose Profile charts for anyone who’s interested.
Since losing the sensor, I’ve been doing paw prick BG tests at 1200 & 2400. BG readings have mostly been 106 and 142, with one outlier of 187. I’m giving alternating doses of 1.0 and 1.5U INS.
Once we resumed MIR a month ago, Candy’s weight began to improve. Daily 1.0mg doses worked better than QOD. She’s now up to about 9.4 pounds, slightly more than when we adopted her.
CGM Questions:
· PLACEMENT: What are good CGM locations? Candy’s first (and only) CGM was placed on her right side, about over her front paw when standing and about 2 inches from the spine. That puts it right over the “crease” at the base of her neck when she’s on her side, with her head up; it seems like it needs to go farther back. How close to the spine can it go? How often can a location be reused?
· ADHESIVE: What supplemental adhesives are people using for CGMs?
· ADHESIVE REMOVER: What do you use to remove the sensor and/or residual adhesive?
· OVER-BANDAGE: What are people’s experiences with over-bandages, to keep the kitty from tearing off the sensor?
· PROTECTIVE VEST: Has anyone found a good vest to protect a CGM? Searches so far turn up “Thunder Vests” (too heavy), “recovery suits” that go over all four legs (too long), and assorted costumes. I’m looking for a light-weight vest-type garment with a Velcro (preferred) or zipper closure in the back that can be worn for extended periods,
Thanks!
Cal