Brenna & Charleston
Member Since 2022
Hello,
Charleston and I (Brenna) had introduced ourselves on the Facebook forum last Saturday (11/5) and have finally made it to our first post on the FDMB. We have been so appreciative of the warm welcome of this community! <3
Charleston is a ~11yo, gorgeous orange tabby who is blind. My husband and I adopted him in August 2021, after he had been found on a road in NM severely beaten up--the rescue thinks an animal attacked him. He is my ever vigilant coworker and study partner full of sooo much love. Since we have had him, the poor fellow has had a rodeo of health occurrences (CKD diagnosis, removal of his remaining eye (glacoma), removal of his remaining teeth (stomatitis), high blood pressure (regulated w/ Amplodipine), hip arthritis, discovery of a heart murmur, and now diabetes). All that being said, he remains the gentlest, loving spirit I have ever known who finds joy in Colorado sunshine, walking through grass and crinkly paper, and snuggling galore.
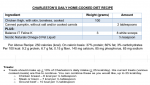
With diagnosis on Friday, 11/4, I immediately started home testing on Saturday with the ReliOn Premier meter. Our vet still stands firm on the viewpoint of fasting for 12 hours and feeding two massive meals with the high recommendation of kibble (massive for Charleston, I've only ever seen him be able to eat ~65 kcal in one sitting). I did a trial of the vet's recommendation for one cycle and will not be continuing with the 12 hr fasting given the stress it put Charleston through. I am quietly searching for another vet to work with (but have also shared a link to my spreadsheet with our current vet. Perhaps our data will speak for itself and we can continue onward working together--this will be determined later this week). I am maintaining a LC Wet diet and feed throughout the day (at PS, as well as what seems to be averaging to +4/+8). Charleston is underweight so I typically feed when he is hungry. Of important note, at diagnosis, I did switch Charleston to an LC wet diet. Prior to diagnosis, he typically had kibble to graze on throughout the night and had been eating Royal Canin Renal D, T, & S for the past two months (he commonly shifts what he likes to eat as is typical for a cat with CKD).
The vet asked us to administer Glargine if he only eats 1/2 of the PS meal (67.5 kcal) or 1.0u for a full meal PS (137.0 kcal). As mentioned earlier, Charleston will not eat large amounts in one go--however, he has been meeting his daily calorie needs by feeding throughout the day. To be safe and given the diet change to LC, I have been following the lower dosing direction of 0.5u while feeding throughout the day. (On a sidenote, my husband and I had been car traveling with Charleston the week prior to diagnosis. I can't help but wonder if we accidentally stressed his poor body to the limit and contributed to high glucose).
My question: I am trying to remain calm and patient. With Charleston having CKD, I would like to be as proactive as possible to prevent kidney damage from high glucose. He has not had ketones in his urine. I conducted a curve on Day 5 and Day 6 after first administration of insulin (missed one data point on accident for Day 6). Given his consistency in the 200's and the vet's prescribed desire of 1.0u as a full dose (2x daily), what is your experienced opinion on if I were to bump his insulin dose up to 0.75u? Am I acting too soon? Perhaps I need to give the diet change and data collection more time?
With appreciation,
Brenna & Charleston
Charleston and I (Brenna) had introduced ourselves on the Facebook forum last Saturday (11/5) and have finally made it to our first post on the FDMB. We have been so appreciative of the warm welcome of this community! <3
Charleston is a ~11yo, gorgeous orange tabby who is blind. My husband and I adopted him in August 2021, after he had been found on a road in NM severely beaten up--the rescue thinks an animal attacked him. He is my ever vigilant coworker and study partner full of sooo much love. Since we have had him, the poor fellow has had a rodeo of health occurrences (CKD diagnosis, removal of his remaining eye (glacoma), removal of his remaining teeth (stomatitis), high blood pressure (regulated w/ Amplodipine), hip arthritis, discovery of a heart murmur, and now diabetes). All that being said, he remains the gentlest, loving spirit I have ever known who finds joy in Colorado sunshine, walking through grass and crinkly paper, and snuggling galore.
With diagnosis on Friday, 11/4, I immediately started home testing on Saturday with the ReliOn Premier meter. Our vet still stands firm on the viewpoint of fasting for 12 hours and feeding two massive meals with the high recommendation of kibble (massive for Charleston, I've only ever seen him be able to eat ~65 kcal in one sitting). I did a trial of the vet's recommendation for one cycle and will not be continuing with the 12 hr fasting given the stress it put Charleston through. I am quietly searching for another vet to work with (but have also shared a link to my spreadsheet with our current vet. Perhaps our data will speak for itself and we can continue onward working together--this will be determined later this week). I am maintaining a LC Wet diet and feed throughout the day (at PS, as well as what seems to be averaging to +4/+8). Charleston is underweight so I typically feed when he is hungry. Of important note, at diagnosis, I did switch Charleston to an LC wet diet. Prior to diagnosis, he typically had kibble to graze on throughout the night and had been eating Royal Canin Renal D, T, & S for the past two months (he commonly shifts what he likes to eat as is typical for a cat with CKD).
The vet asked us to administer Glargine if he only eats 1/2 of the PS meal (67.5 kcal) or 1.0u for a full meal PS (137.0 kcal). As mentioned earlier, Charleston will not eat large amounts in one go--however, he has been meeting his daily calorie needs by feeding throughout the day. To be safe and given the diet change to LC, I have been following the lower dosing direction of 0.5u while feeding throughout the day. (On a sidenote, my husband and I had been car traveling with Charleston the week prior to diagnosis. I can't help but wonder if we accidentally stressed his poor body to the limit and contributed to high glucose).
My question: I am trying to remain calm and patient. With Charleston having CKD, I would like to be as proactive as possible to prevent kidney damage from high glucose. He has not had ketones in his urine. I conducted a curve on Day 5 and Day 6 after first administration of insulin (missed one data point on accident for Day 6). Given his consistency in the 200's and the vet's prescribed desire of 1.0u as a full dose (2x daily), what is your experienced opinion on if I were to bump his insulin dose up to 0.75u? Am I acting too soon? Perhaps I need to give the diet change and data collection more time?
With appreciation,
Brenna & Charleston